Code Calls
If you need to put out a code then the hospital emergency number is 777.
It is expected that a registrar will attend all codes as required. If you are unable to attend (e.g. placing a line) then you must ensure that one of your colleagues can attend. If you will be undertaking an uninterruptible task then please have one of your colleagues hold the emergency pager and your phone until you are free again.
The DCCM registrar attends codes within the hospital and emergency department except on the 3rd and 4th floor. Codes on the 3rd and 4th floor are covered by the CVICU registrar.
If there is more than one code on the wards then a second code team may be called. If the second code team is called for the 3rd and 4th floor then please attend this code and manage the patient as appropriate. In general if escalation is required for those patients then this will occur via discussion with the CVICU consultant however if this is not clear then please discuss this with the DCCM consultant. If a second code call has been put out and the DCCM registrar has in fact completed with the first code call then please attend the new code.
If you are busy at an emergency in another part of the hospital and unable to attend a code then please phone one of your colleagues and ask them to attend in the first instance.
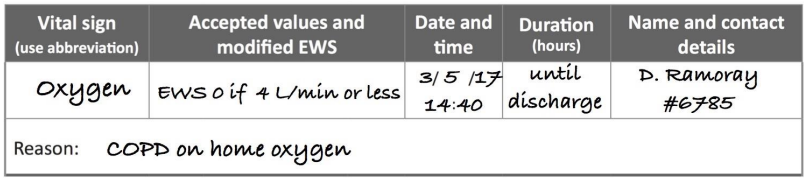
There are a number of different types of code calls in Te Toka Tumai. Below are the most common codes that you will be expected to attend along with the other team members that will also receive the code.
Code Blue
Code Blue is for patients who have a cardiac or respiratory arrest.
Code Red
Code Red is for patients who have a medical emergency (excluding cardiac or respiratory arrest). This can include scoring highly on the NZ Early Warning Score (NZEWS) or due to clinical concern. Patients who have a code red may deteriorate to a code blue.
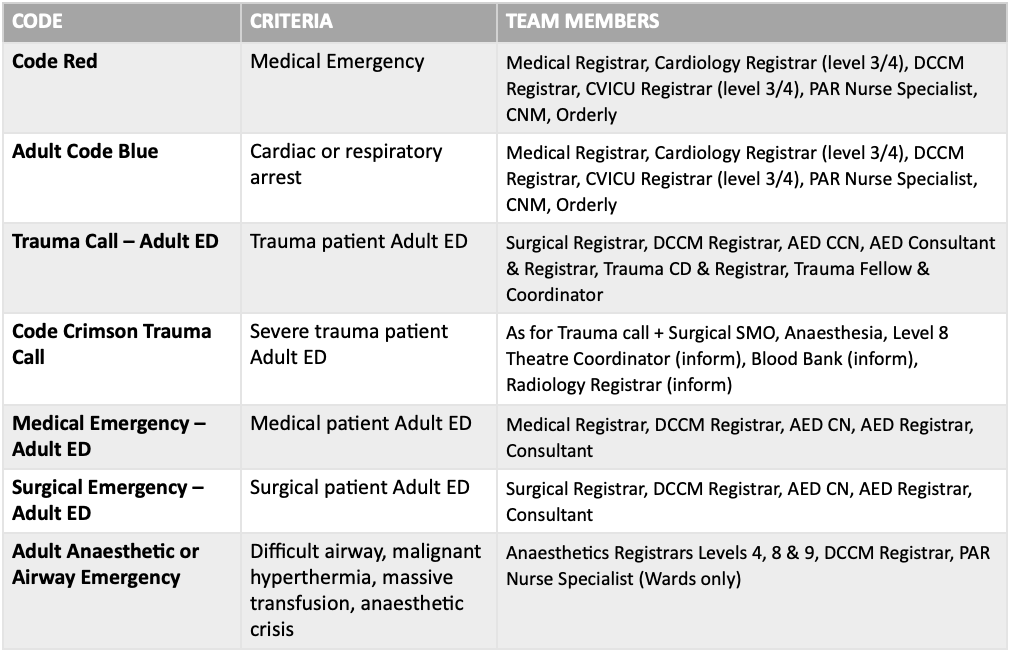
Trauma call
A Trauma call is placed by the Emergency Department when a patient with severe trauma is expected or has arrived. This call is often put out on the basis of the R40 call from the ambulance service and information is often limited initially.
These patients will usually be in the resuscitation area in the emergency department. On arrival in the resuscitation area please introduce yourself to the team leader and assist with the patient. There are pre-printed labels with designated roles and a place for your name which you can use. These can be used over PPE if required.
A discretionary trauma call may be on the basis of mechanism, physiology, co-morbidities or a combination of these. It should especially be considered for an elderly patient.
Code crimson
This is an activation of additional staff for critically ill trauma patients who are highly likely to require urgent surgery, interventional radiology and imaging and/or a massive haemorrhage protocol (MHP).
In a code crimson the Surgical SMO, anaesthesia, Level 8 theatre co-ordinator, radiology registrar, and blood bank are also informed.
Criteria for Code Crimson
Meets criteria for a standard Trauma Call activation on R40 (pre hospital notification) or at any time while in the Adult Emergency Department (ED).
PLUS
An Assessment of Blood Consumption score (ABC) score of two (2) or more.
OR
The Trauma Team Leader feels the patient is likely to require an urgent operative or interventional radiological intervention.
Airway emergency
The purpose of the Airway Emergency Call is to provide timely anaesthetic support staff, to an Auckland City Hospital adult anaesthetic or airway crisis, when local support is not available or additional support is needed.
This may be placed by any staff member in the event of crisis (e.g. difficult or failed airway). If this occurs in DCCM then direct one of the team members to phone 777 and state “Adult Anaesthetic Emergency” along with the location.
PAR service
The Patient at Risk (PaR) team was established in July 2017, in response to growing evidence supporting the use of Critical Care Outreach.
The team provide a 24 hour service aimed at assisting in the management of deteriorating patients on wards, focussing on early patient assessment and timely intervention by providing independent recommendations.
Simultaneously, the team liaises and collaborates with wider multidisciplinary team to ensure patients receive appropriate assessment, timely management and on-going surveillance.
NZEWS
The New Zealand Early Warning Score (NZEWS) provide a safety net for adult patients who acutely deteriorate while in hospital. The New Zealand early warning score (NZEWS) is calculated from routine vital sign measurements and increases as vital signs become increasingly abnormal. The EWS triggers an escalating clinical response so that clinicians with the right skills can intervene and manage the patient’s deterioration.
The national vital signs chart and NZEWS were developed based on the best available human factors and clinical evidence and tested for usability in a number of different hospital sites and ward settings. These included acute tertiary medical and surgical wards, inpatient mental health units, a private surgical hospital, and small regional hospitals.
The NZEWS relies on clinicians monitoring and documenting seven core vital sign parameters within the graphing area (section 1) of the chart. These are:
respiratory rate
oxygen supplementation
oxygen saturation
heart rate
blood pressure
temperature
level of consciousness.
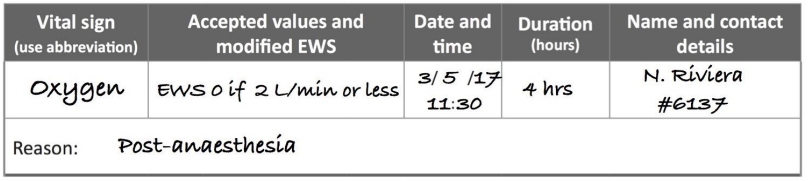
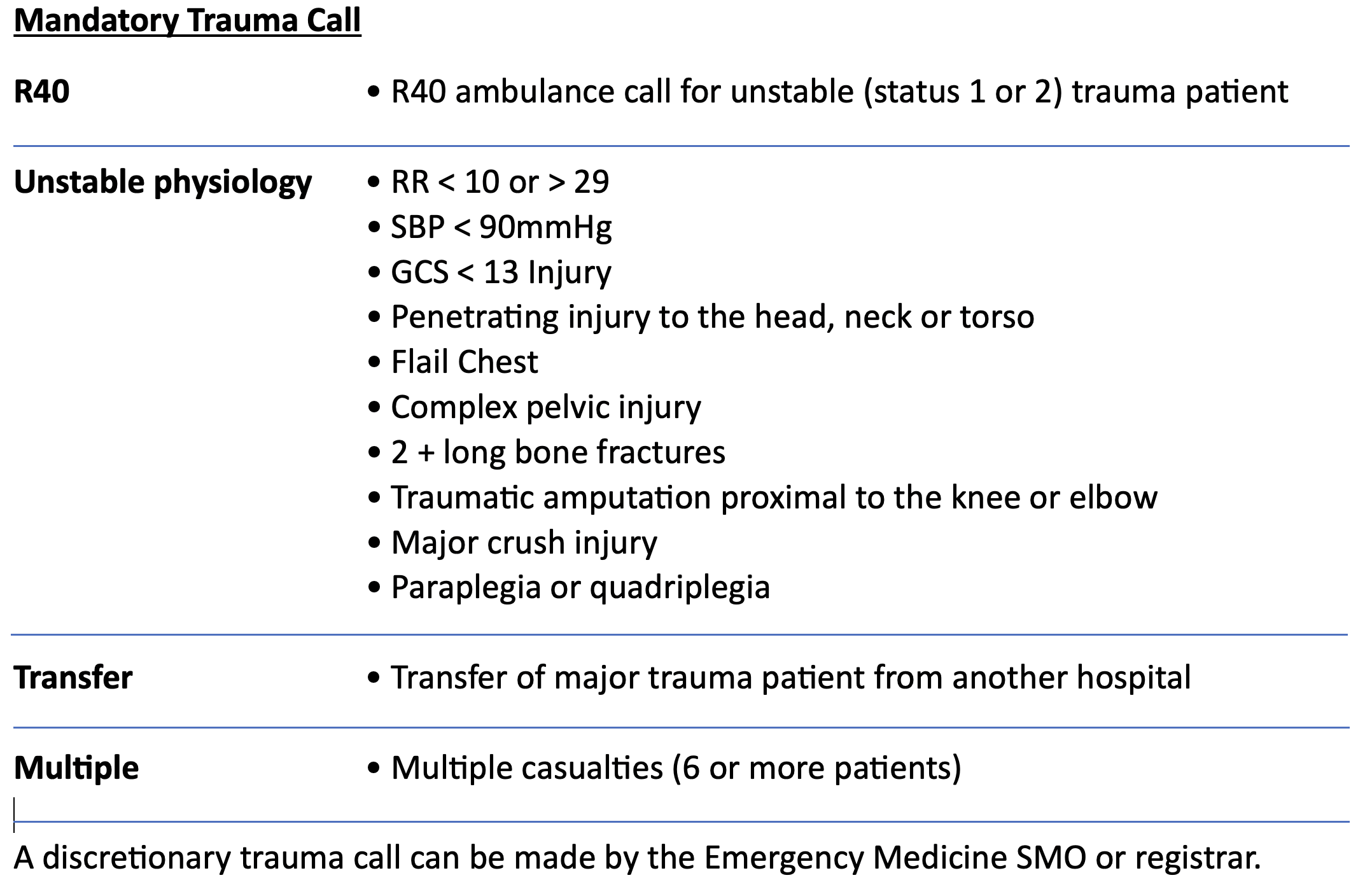
Modifications may be made to the NZEWS triggers for individual patients when chronic disease, drug therapies, or other factors cause their vital signs to fall outside of the normal range on the national vital signs chart.
When making modifications the clinician must consider the clinical risk to the patient if vital sign abnormality is normalised. Clinical risk can be mitigated by ensuring modifications are discussed with a senior clinician and reviewed at regular intervals so they remain appropriate as the patient’s condition changes. The duration of all modifications must be documented to ensure that timely clinical review is undertaken.
Appropriate modifications are shown below.