Medications
Please refer to the section on drug charting Expectations - Drug Charts.
Commonly used antibiotics – Script App
Te Toka Tumai has guidance on antibiotic prescribing which is available via the Script application.
To download this please visit your mobile devices application store and search for “Script – ADHB guidelines” application. The publisher is listed as Auckland District Health Board.
This application provides local information and guidance of antibiotic prescribing. There are times when it will be appropriate to deviate from these guidelines especially in intensive care patients. In particular patients in the ICU often have altered clearance due to renal impairment or renal replacement therapy.
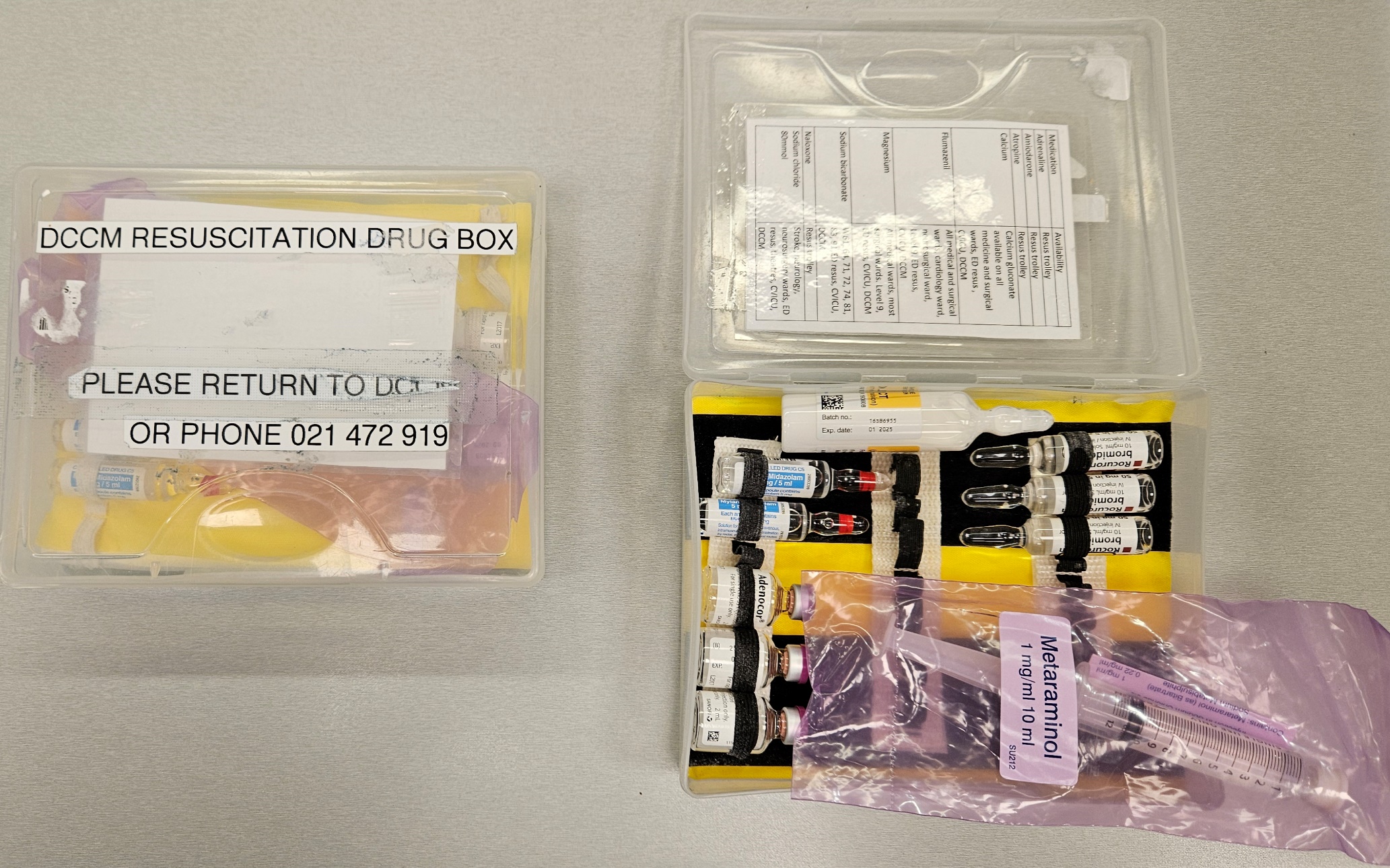
Resuscitation drug box
The resuscitation drug box is a small plastic box which contains medications which are otherwise difficult to access in a timely fashion during an emergency call.
There are 3 resuscitation drug boxes and they are located in the central fishbowl. When you attend a code on the ward then please take this box with you. At the end of the code then please bring it back to the ICU.
On the rear of the box you will find a list of the medications. If you use any medications then it is your responsibility to restock the box. This can be done with medications from of the drug rooms on DCCM.
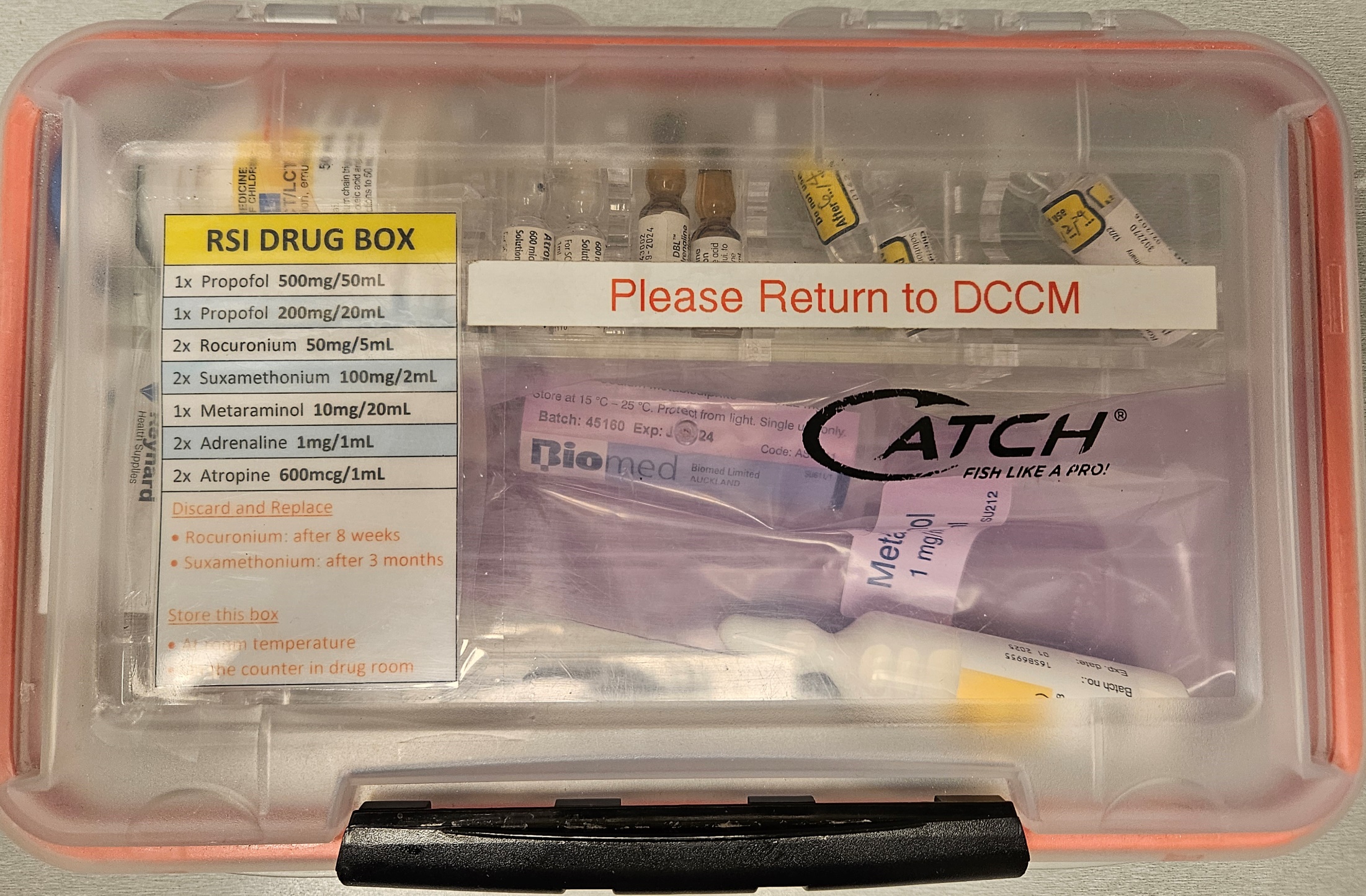
Intubation drug box
In each of the drug rooms underneath the controlled drug safe there are a number of boxes containing intubation drugs.
If a patient requires intubation then you can ask for one of the team members to obtain this box for you. Please note that this does not contain any opiates and you will need to request opiates separately.
If you draw up drugs for intubation then use the prelabelled stickers if they are available.
VTE prophylaxis
Venous thromboembolism (VTE) may contribute up to 12% of deaths in ICU and is a preventable cause of hospital death. Both asymptomatic and silent VTE is common in medical and surgical patients including those in the ICU.
In DCCM we routinely use a variety of non-pharmacological techniques (including the use of intermittent pneumatic compression devices and early mobilisation) and pharmacological techniques in patients to minimise the risk of VTE. If patients are not at significant risk of bleeding then they will usually receive either enoxaparin or subcutaneous heparin (5000units q8h or q12h).
Neurosurgical patients are also able to receive VTE prophylaxis and can be expected to have similar benefits in the prevention of VTE. Specific guidance on this patient group is available in the Standard Operating Policies (see section 0).
Fluids
Fluids containing predominantly water and little or no sodium are titrated to osmolality, and serum sodium concentration is used as a surrogate measure of osmolality. The preferred fluid in most patients for maintenance is 5% glucose.
Crystalloids are preferred over colloids for expansion of intravascular volume, unless a colloid is specifically clinically indicated.
In patients following renal transplantation then a balanced crystalloid (Plasmalyte-148) is used for replacement of losses and for fluid boluses as required.
Further details regarding intravenous fluid therapy may be found in the Standard Operating Policies.