Common ICU Problems
Delirium
Delirium is common in the intensive care, characterised by an acute onset of fluctuating levels of consciousness, cognition and perceptions. Approximately half of our ventilated patients develop delirium. Delirium is associated with increased ICU stay, and higher morbidity and mortality.
Less than a third of delirium is recognised in hospitalised older adults (Marcantonio 2017). Without the use of a structured diagnostic tool delirium is often undiagnosed in the critically unwell (Reade et. al 2014).
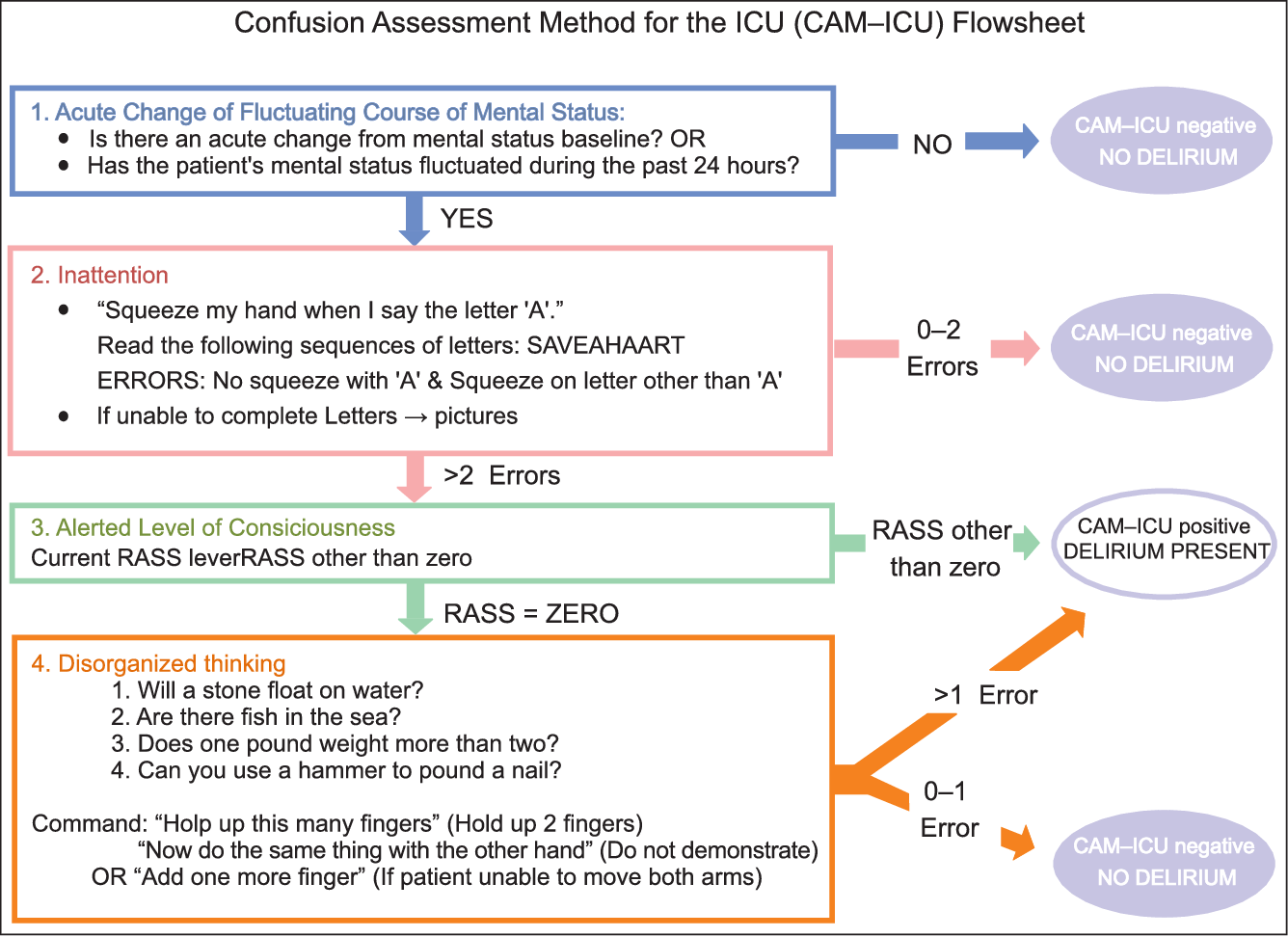
Delirium should be assessed for every shift by nursing staff, or more frequently if there is suspicion of change, using the Confusion Assessment Method for the ICU (CAM-ICU). This is a validated screening tool for delirium in the critically unwell and can be used on all adult intensive care patients with a Richmond Agitation and Sedation Scale (RASS) of greater than -3/moderate sedation (The RASS can. The CAM-ICU is the most widely used and specific of the screening tools for delirium in ICU, and has excellent reliability (Ely et. al. 2001, Sherpa et. al 2012).
The CAM-ICU establishes the presence of delirium based on the presence or absence of four factors related to attentiveness and disorganised thinking as described in the flow sheet below.
The patients’ physical environment plays a part in preventing delirium, though evidence for any one intervention is generally poor (Devlin et. al. 2018, Herling et. al.2018).
The presence of delirium does not mandate the prescription of an antipsychotic. The evidence for pharmacotherapy for delirium is generally poor. Neither typical nor atypical antipsychotics are associated with shorter duration of delirium (Burry et. al 2018). The focus should be on non-pharmacologic management. Drug therapy is reserved for patients who are unsafe or who have distressing symptoms (Devlin et. al. 2018).
Delirium may be:
Hyperactive – agitation, hypervigilance, irritability, lack of concentration, and perseveration
Hypoactive – diminished alertness, absence of or slowed speech, hypokinesia, and lethargy
Mixed – a mixture of hyperactive and hypoactive features
Hypoactive delirium can be difficult to diagnose in the intensive care unit due to the presence of confounding features such as medications.
Additional information on delirium including suggested medication dosing for appropriate patients can be found in the Standard Operating Policies.