Expectations
Teams
Due to the number of patients in DCCM we function in 2 pods. These are labelled as the Red and Blue pods. During the day there will be a consultant and a registrar assigned to each of the teams. Each team will have responsibility for 6-14 patients on most days. The Blue team will have a greater proportion of patients who are predicted to have a longer stay in intensive care and the allocation of both the consultant and registrar aims to provide some continuity for these patients. The Red team will have a greater proportion of patients with a shorter predicted stay in intensive care. This includes more of the elective post-operative patients.
The red and blue patients are not separated geographically. In order to determine if a patient is on the Red or Blue team then you can consult the patient board in the main corridor or refer to the daily handover sheet.
Although there are separate teams there is an expectation that paperwork and other tasks will be shared between the teams as needed to both ensure that these are completed in a timely fashion and also to balance any workload issues.
There is also one registrar whose primary role is to attend code calls and patient reviews. This role is referred to as the Out registrar or Yellow registrar. If they are not attending patients in other areas of the hospital then they are based in the intensive care unit and will perform tasks and paperwork as required.
Bloods
Blood tests in DCCM are requested by the medical team and usually taken from either an arterial line or central line by the nursing staff. If a patient does not have a central or arterial line then a peripheral blood sample will be required.
Blood tests are ordered on the 24 hour chart. Blood tests and CXR for the following day can be requested at the top right corner of the 24 hour chart. These will be taken between 5am and 6am in order to ensure that they are available for the morning ward round. The night registrars will review these results once available (this is usually between 7am and 8am), intervene on any clinically significant results, and note them on the 24 hour chart for the upcoming day. Other blood tests can be requested on the bottom edge of the 24 hour chart, this includes arterial blood gases or blood glucose. The nursing staff will send these at the requested times and complete the request form however it is your responsibility to review the results and act upon these as appropriate. For less frequently ordered tests then please write out the blood form yourself and advise the nursing staff.
Not all nursing staff are able to take bloods so if the patient does not have ana arterial or central line then you may need to take these bloods yourself if an appropriately trained nurse is unavailable. This also applies to blood cultures. We do not routinely take blood from arterial lines or central lines other than at the time of insertion.
Some of the nursing staff are able to take blood tests or insert IV lines but you will need to check with the individual nurse caring for the patient. If the nurse is unable to take a peripheral blood sample then this is the registrars responsibility.
X-rays
X-rays are requested on the “Orders” tab on Regional Clinical Portal. This tab is available once you select a patient.
On the daily ward rounds we will discuss if an X-ray is required for the following day. X-rays are not routine but rather are performed for clinical indications. If a patient requires an X-ray for the following day then please order this via the Regional Clinical Portal. The radiographers will perform an X-ray round in the morning. This starts at approximately 7am and requests should be completed before this (requested by the night registrar).
Ward round and daily schedule
The usual daily schedule looks something like this:
0800 Paper handover from night team to day team in the fishbowl.
0830 Ward round
1030 Daily review of radiology in the department
1600 Afternoon ward round
2000 Evening registrar handover
2100 Evening ward roundOn Tuesday and Friday there is an Infectious Diseases team meeting in DCCM at 1130.
On Tuesday there is registrar teaching from 1330 to 1530. During this time please handover your phone/pager to the consultant who you have been working with on that day. The Yellow/Out registrar will hand their devices to the consultant in the backup role for the day.
Documentation
The consultant will complete a daily note on patients in DCCM. This note is not completed for patients on the day of admission or the day of discharge as the admission and transfer summary is felt to contain similar information. If a patient is bed-blocked then they will not always receive a consultant note. These notes are available on the Regional Clinical Portal. Some patients will benefit from having their progress documented in the written clinical record and these entries should be dated and timed in the usual fashion.
Daily plans for the patient are documented on the 24 hour chart at the patient bedside.
Procedures including intubation, central line insertion, chest drain insertion, and tracheostomy insertion should be documented in the patient record. Intra-hospital transfers may be documented in the patient record. This must occur if there were any complications or concerns during transfer. There is a separate Intra-hospital transfer document which is completed by the nursing staff.
If you update whanau or friends then please document this in the clinical record along with what was discussed.
Transfer notes
On transfer to the ward a transfer summary is required for the patient. You can find this under the EDS tab on Regional Clinical Portal. If the patient is being discharged (transfer to another hospital or directly home from DCCM) then they will require a Discharge Summary which can also be found under the EDS tab. Please ensure That you select the correct episode number when writing transfer and discharge summaries.
The transfer note should contain a summary of the admission in DCCM and will facilitate a good handover of relevant patient information.
A drug chart should be completed in addition with the transfer summary (see below).
Drug charts
In DCCM
In the Department of Critical Care Medicine drugs are prescribed on the “DCCM Treatment Sheet”.
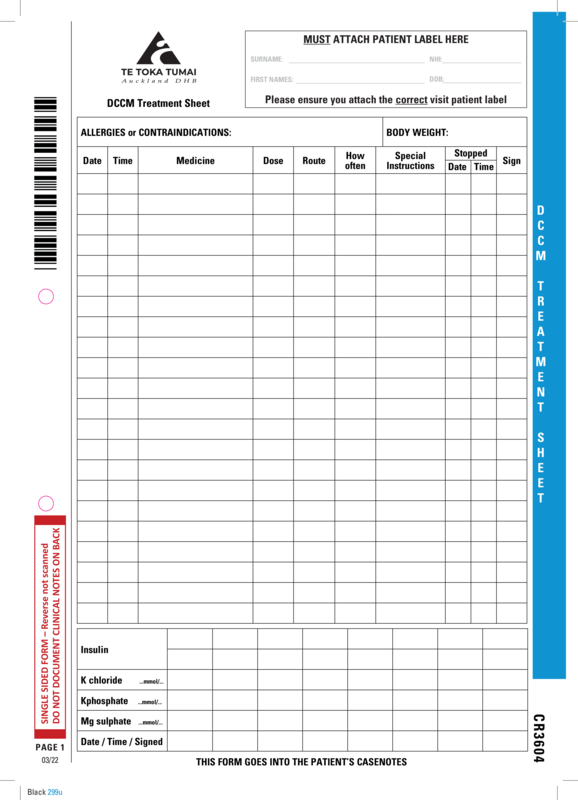
Please keep the following points in mind when prescribing drugs for patients:
All drugs are to be charted legibly. Consider using capital letters and printing.
Prescribing in the DCCM is generic. Common medications which sometimes cause confusion include amoxicillin/clavulanate (Augmentin), enoxaparin (Clexane), and oxycodone.
If you are prescribing controlled release medications then please ensure that this is noted on the drug chart e.g. Oxycodone CR.
The allergies and contraindications section should be completed. If the patient is unable to respond and this information is unable to be obtained from the clinical notes or family members then please write “Unknown” in this section.
If antibiotics are prescribed then these should have an indication documented along with a treatment length. If you are unsure of the appropriate treatment length then please discuss this with a consultant. Review dates are also acceptable in relation to antibiotic duration.
In the How often column please indicate the frequency. We have a strong preference for this to be prescribed in reference to hours due to the increased precision. For example use “q12h” rather than BD. If a medication is required to be given at a particular time then please write this in the Special Instructions column.
Not all of a patients regular medications will be required to be charted when first admitted to DCCM. In particular anti-hypertensives are often withheld, particularly in patients who may become hypotensive.
Medications with daily dose adjustments (e.g. gentamicin) should be documented in the ICU medication chart section for regular medications (e.g. Gentamicin as per trough levels), and then charted as stat doses as required (e.g. Gentamicin 360mg IV).
Medications that have separate prescription charts (e.g. Warfarin, epidural infusions, heparin infusions and patient controlled analgesia) must be documented in the section for regular medications (e.g. Morphine as per PCA chart).
When re-charting antibiotics and other medications, transcribe the start date and date for review to the new drug chart.
On transfer to ward
On the transfer of a patient to the ward a National Medication Chart will be required. Please complete this along with the transfer summary. This is a good opportunity to review the patient medications and ensure that appropriate medications for the ward are prescribed. If a patient is being transferred to another hospital then a medication chart will not be required however the discharge summary should include a complete list of medications along with dosing intervals and timing of last dose if required.
Detailed Order Sheet
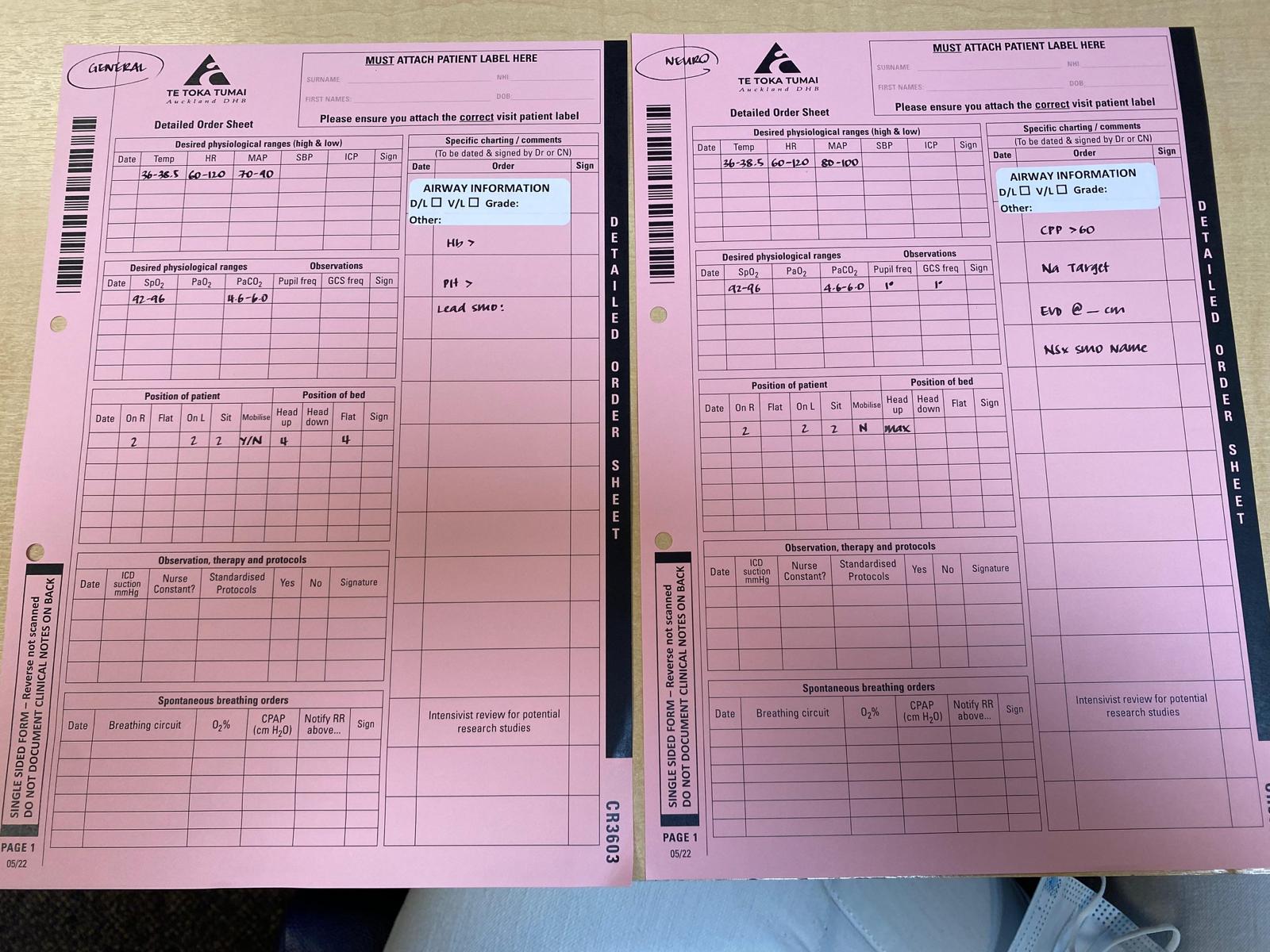
The detailed order sheet is a part of our documentation where we record desired physiological ranges, frequency of observations, airway information including grade of intubation, the use of suction for chest drains, frequency of type of turns, and other relevant information including the neurosurgical SMO for neurosurgical patients.
Please ensure that this is completed when the patient first arrives in DCCM. Examples for a general patient and a neurosurgical patient are below. Please note that these are examples only and that the physiological parameters will depend on the underlying patient co-morbidities, diagnosis, and progress.
Hand hygiene
Hand hygiene with either alcohol gel or hand washing is a key measure in preventing nosocomial infection. Regular audits are undertaken to provide feedback on compliance with hand hygiene targets. Please feel free to remind other staff about this when appropriate.